Medicaid Fraud Fallout: Crump Blasts Arizona's 'Witch Hunt' Against Healthcare Providers
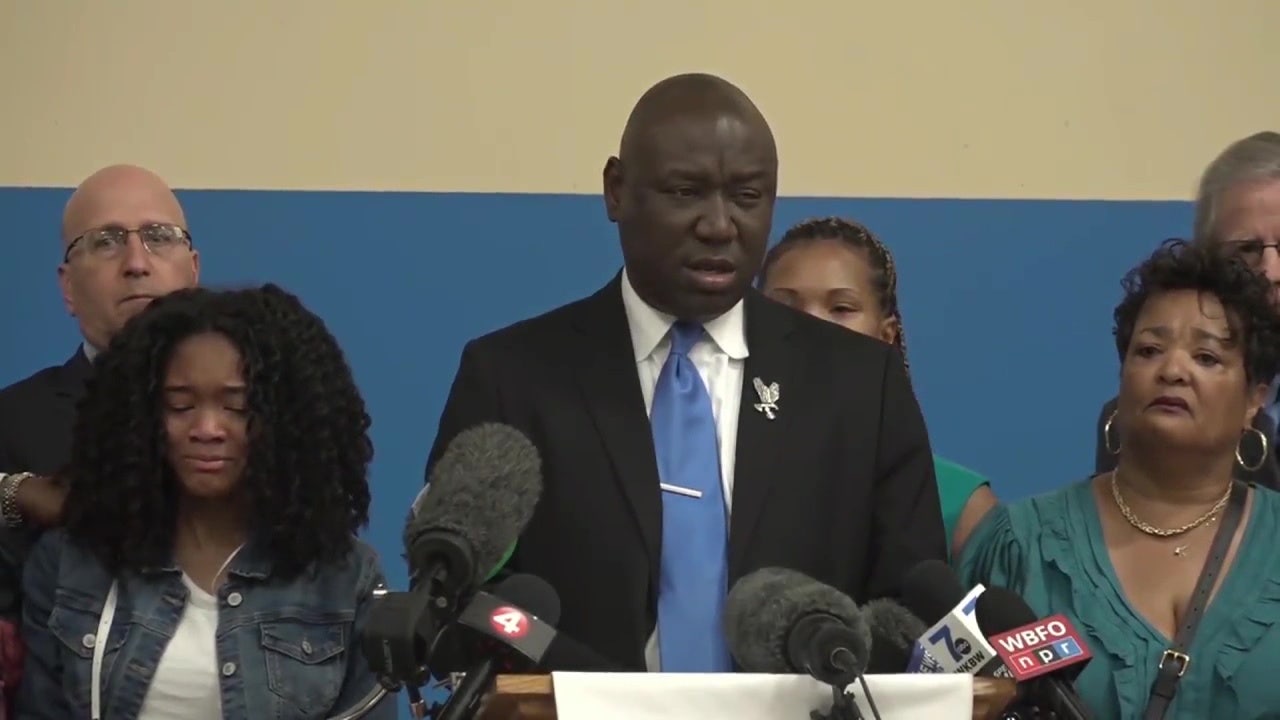
Civil rights attorney Ben Crump is diving deep into Arizona's massive Medicaid fraud scandal, which allegedly siphoned off nearly $2 billion from state healthcare funds. Known for taking on high-profile cases that expose systemic injustices, Crump is bringing his legal expertise to unravel what could be one of the most significant healthcare fraud investigations in recent Arizona history.
The scandal, which has sent shockwaves through the state's healthcare and political landscape, involves complex allegations of fraudulent claims and financial misconduct within the Medicaid system. Crump's involvement signals a potentially transformative legal battle that could not only seek financial restitution but also push for comprehensive reforms in state healthcare administration.
With his track record of holding powerful institutions accountable, Crump's entry into the case suggests a thorough and potentially groundbreaking investigation that could have far-reaching implications for Arizona's healthcare infrastructure and public trust in government-managed health programs.
As details continue to emerge, stakeholders and citizens alike are watching closely to see how this legal challenge will unfold and what consequences it might bring for those allegedly responsible for the massive financial discrepancies.
