Healthcare Shortchanged: How Connecticut's Community Clinics Are Falling Through the Funding Cracks
Community Health Centers are the lifeline of healthcare for millions of Americans, yet current policies are undermining their ability to provide quality, accessible medical care. The misguided approach of artificially reducing funding creates a dangerous illusion of cost savings that ultimately hurts the very patients these centers are designed to serve.
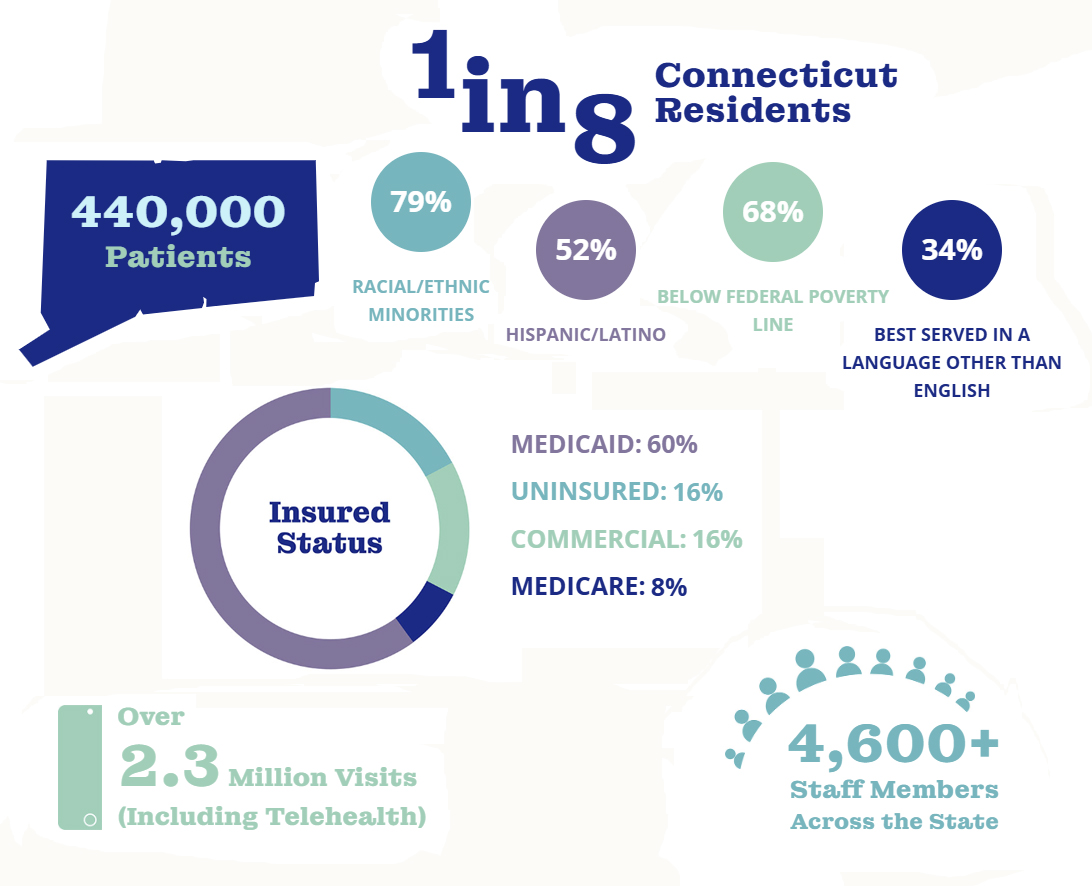
These critical healthcare facilities operate on razor-thin margins, serving vulnerable populations in underserved communities. By implementing restrictive funding mechanisms, policymakers are effectively choking the resources that enable these centers to deliver essential medical services. What might seem like a budget-cutting strategy actually results in increased long-term healthcare costs and reduced access to preventive care.
The real cost of these shortsighted policies goes far beyond simple budget lines. When Community Health Centers are forced to scale back services, limit staffing, or close entirely, patients are left without critical medical support. Rural and low-income communities suffer the most, facing increasingly limited healthcare options and potential health crises.
It's time to recognize that investing in Community Health Centers is not an expense, but a smart, strategic approach to maintaining public health. By providing adequate funding and support, we can ensure these vital institutions continue to serve as healthcare safety nets for our most vulnerable populations.
